Stent-based treatment for aortic dissections
Problem statement
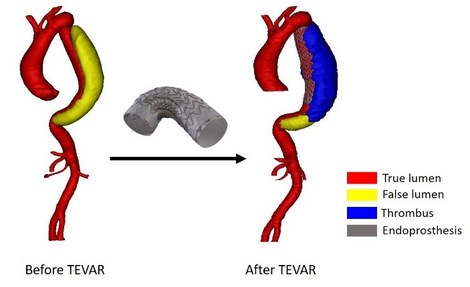
Towards a computational framework for TEVAR in type B aortic dissections
Starting from a database including CT scans of 96 patients with a type B aortic dissection, of whom 45 were treated with TEVAR, idealized as well as patient-inspired 3D geometries of type B aortic dissections are developed. This database was collected in collaboration with the university hospitals of Ghent and Düsseldorf. The geometrical information is used as starting point for the models representing the acute and long-term effects. Although the long-term effects are essential in assessing the benefit of TEVAR for a particular patient, the current focus of the research project is to set up the models that represent the acute effects of the treatment. In particular, models for the stent-graft deployment, the blood flow, the dissected aortic wall, as well as their interaction, are being developed. Hereby, particular attention is given to the robustness of the models. Indeed, it is the aim that the usage of the model set-up is not limited to a few patient-specific geometries, but that the models can be used for a broad range of patients with a type B aortic dissection. Moreover, assessing the sensitivity of multiple assumed model parameters is one of the essential steps in developing a reliable computational model. Therefore, parametric models were created. The first steps of the modeling process were taken in idealized geometries.
A simplified parametric model of an aortic dissection has been set up. Although the geometry, developed in pyFormex, is strongly simplified, it contains the main features of an aortic dissection, being the false lumen and multiple tears. While an idealized geometry has been used, an advanced hyperelastic anisotropic material model was included for the aortic walls. The finite element analyses were performed in Abaqus.
A finite element model of the stent-graft deployment, is currently under development. The deployment of a self-expanding one-ring stent has been studied extensively. Some initial steps have been taken towards the expansion of a stent in a dissected wall model, wherein the tissue is assumed to be isotropic and hyperelastic. As an illustration of the technical possibilities, an animation of the stent-graft deployment in an aneurysm model, developed by Dr. Sander De Bock, is shown in figure 2.
Starting from a similar geometry as the one of the aortic wall model, a computational fluid dynamics model of the blood flow has been set up, using Fluent. With the future perspective of going towards a fluid-structure-interaction model, the blood flow is modeled using overset meshes. This technique allows large displacements of the aortic wall and the dissected membrane during the cardiac cycle without the need to adapt the fluid domain during the simulation.

In conclusion, initial steps have been taken for the three models required to predict the acute effects. Future work will be situated in assessing the sensitivity of the models and increasing the geometrical complexity in order to progress towards a patient-specific setting. The interaction between the different models will be taken into account as well.
IBiTech researchers currently active on the project
Funding sources
- Doctoral grant strategic basic research (1S48920N) of the research foundation-Flanders (FWO-Vlaanderen)
- Grant research project (G086917N) of the research foundation-Flanders (FWO-Vlaanderen)